
Breathing and thoracic mobility are intrinsically linked. Are you tapping into the benefits of breathing?
“Breathing is the first act of life and the last. Our very life depends on it.”
This is a famous quote from Joseph Pilates. It is estimated that 10% of the population suffers from breathing pattern dysfunction, and this proportion increases to 83% among those who suffer from anxiety. We have long recognized that slowing the breath via parasympathetic breathing can help to slow the mind and manage anxiety.
But what about breathing for mobility? Aside, from slowing the mind, breathing also facilitates movement and can be a valuable tool to address mobility issues. The rib cage is one of the biggest areas of restriction in the thorax and in turn, certainly has an effect on thoracic mobility. One of the best ways to distract the rib cage and unlock movement in the thoracic spine is to breathe. That said, here is why it is important to understand how we need to be breathing to unlock mobility.
Enjoyed this video? Make sure to subscribe to our YouTube channel!
MOBILITY DEFICITS
Mobility deficits typically stem from problems that are either more mechanical, chemical or neurological, or a combination of these.
By mechanical problems I am referring to joint or soft tissue restrictions – these are the most treated issue and most common way in which people address mobility problems. It is why many people have recourse to manual therapy and utilize various forms of self-myofascial work.
Chemical-type problems are things like inflammation, ischemia, and poor lymphatic drainage, which can also affect mobility. I suggest you ally yourself with competent professionals in the areas of nutrition and lymphatic therapy that you can refer to if you suspect something going on there. It’s not my area of expertise, so I certainly refer out when I have any doubts. Dr. Perry Nickelston is a chiropractic physician with an interesting approach to lymphatic therapy. There are also massage therapists who specialize in lymphatic drainage.
Finally, mobility deficits can come from a neurological or neuromuscular issue that has nothing to do with joint or tissue restrictions. An easy example is the hypermobile individual who often “feels” tight but has no soft-tissue and certainly no articular restrictions.
An effective mobility strategy needs to cover each of these areas, as focusing on one aspect alone will usually not be sufficient. To reinforce efficient movement patterns, you have to be able to move efficiently. Limitations in movement that come from poor soft-tissue quality are a significant barrier to movement quality and need to be addressed if we hope to move more efficiently. However, there is an active component to mobility that needs to be addressed, because mobility and stability are intrinsically linked. Once we have opened up range of motion, it is imperative to work within that range to gain awareness and control. This is what allows mobility to be maintained in the long term.
I discuss this as well in my blog article Why foam rolling doesn’t improve mobility.
“BELLY” BREATHING?
The intent of « belly breathing” is honorable. The cue to breathe into the belly was simply meant to get people to understand that the breath needs to come down all the way into the abdomen, as opposed to breathing from the chest. However, the term “diaphragmatic breathing” is more appropriate, as the diaphragm should be a prime mover in the breathing pattern.
Although the breath should be deep and travel beyond the chest, the belly is not the only area that should be moving, nor should there be no movement at all through the chest. During inspiration, the diaphragm contracts and moves down into the abdominal cavity. The contraction of the fibers of the diaphragm, which attaches to the lower ribs, creates a horizontal expansion and distracts the rib cage.
Breathing is 3 dimensional, there should be anterior, posterior and lateral expansion of the chest cavity. This 3-dimensional expansion of the rib cage is pretty significant. If you applied a tape measure around an individual’s rib cage, you should see about a 2.5cm difference in circumference from full exhale to full inhale.
BREATHING AND THORACIC MOBILITY
Every breath is a natural mobilization for the spine, provided it is done right. If you take a deep breath in, allow the diaphragm to descend and the chest wall to expand, the thoracic spine will move into extension. As you exhale deeply and relax, the thoracic spine will flex. Exploring this in various positions can contribute tremendously to subsequent thoracic spine mobilizations. Essentially, it is like warming up the spine. As a plus, if you are working with someone who has high stress or anxiety, breathing will help decrease muscle tension prior to working on a mobilization strategy.
When dealing with a very kyphotic client, working into thoracic extension can be quite aggressive. I often suggest starting with thoracic rotation exercises, as these are usually less aggressive and more tolerable. They also give the client a feeling of movement, whereas working in extension usually has them feeling like they are going nowhere, especially if they are quite restricted.
Adding breathing prior to mobilization exercises is likely to make the entire process even more tolerable. Breathing in the child’s pose position is particularly helpful to tease the breath into the posterior thorax, opening up a lot of the rigidity in there. Have the client breathe in the child’s pose for 2 to 3 minutes ( I strongly suggest 3 minutes as the minimum, unless you are really under time constraints) and follow that up with a thoracic extension mobilization exercise. Watch the main video to see how to perform the breathing and T-spine exercises.
When programming breathing for a client, I always suggest they use a breathing app that sets the duration of the inhalation and exhalation. Ideally, you should be capable of slowing your breath down to 10 seconds, so a 5-second inhale and 5-second exhale. If this is difficult for some initially, use a 4-second inhale and exhale and work your way up. For parasympathetic breathing, the exhale should be equal to or longer than the inhale.
The app I use for myself and for my clients is called Respirelax+, which you can download on most smartphones. I have not found an English equivalent yet, but the settings are fairly straight-forward:
NOT JUST MOBILITY, BUT STABILITY TOO…
If you are dealing with an individual who is an inherently bad breather, not only will this affect mobility of the shoulder complex, but also that of the hip complex. This is because insufficient or poorly coordinated activation of the diaphragm can compromise the stability of the spine.
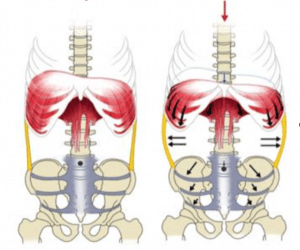
The transversus abdominus muscle (TrA) forms the walls of the thoracopelvic cylinder while the muscles of the pelvic floor and diaphragm form its base and lid (see figure below). This compression cylinder influences the intra-abdominal pressure (IAP) that contributes to the stability of the spine.
If the action of the diaphragm is compromised, the body will look for stability elsewhere, namely in psoas, because they have a direct anatomical connection. I have also seen a lot of apical breathers with hypertonicity in the quadratus lumborum.
As you understand, stretching or soft tissue work for the psoas or QL will only create a change that is short-lived. Incorporating breathing into your mobilization strategy can help address hypertonicity and regulate breathing in the long term. You can also manipulate the positions in which you have your clients breathe to target specific regions. For example, I like to use what I termed “flag pose breathing” (for lack of a better idea for a name) for issues with the QL. The plus side is it also gets into the psoas.
JUST BREATHE
Pilates also once said: “It is tragically deplorable to contemplate the millions who have never mastered the art of correct breathing.” In today’s fast-paced world of high stress and heavy lifting, stress is highly prevalent and can sometimes affect us in ways in which we are not even aware. The neck, sternum, rib cage and thoracic spine are all areas where many people hold their stress. Breathing mechanics at rest is not something most people take the time to notice or work on.
Optimal breathing provides a natural mobilization of the rib cage and spine that is crucial for both mobility and stability. Understanding how breathing can influence the spine, the shoulder complex and the hip complex is another step towards building efficient interventions for mobility that extend beyond just soft tissue release and joint mobilizations.
Consider making breathing part of your intervention if you are looking to improve thoracic mobility, or if you notice that your client does not have an optimal breathing pattern.
References:
Courtney R. The function of breathing and its dysfunctions and their relationship to breathing therapy. Int J Osteop Med 12: 78–85, 2009.
Enjoyed this article? Click the link on the top right-hand corner of the video to share it, we sure do appreciate it!

Mai-Linh Dovan M.SC., CAT(C)
Certified Athletic Therapist
Founder of Rehab-U





Be part of the conversation